And he continues, "I've never had a Black boss. I played football from middle school through senior year of high school and only had one Black coach in that whole time. Not just head coaches, I'm talking about assistants and position coaches. I've had two Black teachers in my entire life. One was for my Harlem Renaissance class, and one was for my sign language class. I've never been to a Black doctor, or a Black dentist. I've never been pulled over by a Black police officer. What I'm trying to explain is that, in 31 years, I've seen three Black people in a position of authority.".
While the theme of racial discrimination is somewhat outside the scope of this blog, July is National Minority Mental Health Month and I think, more than ever, that it's crucial to talk about it. Racial attacks and protests have become routine on media vehicles. Being a white, green-eyed woman has always put me in a rather privileged condition and I can honestly say I never experienced racism first hand in America despite my Latino background. Having the letters "MD" after my name certainly helped.
But, in my profession, I get to feel the pain of people who didn't have the same "luck" to receive fair, equal treatment; who didn't get to have the benefit of the doubt; who have to teach their children to protect themselves from the very ones who were supposed to protect them; who were denied opportunities simply because of the color of their skin. Day after day, I see the tears, struggles and challenges of those black women with mental illness-- a triple minority of an unjust society.

"But what does one's complexion have to do with mental health?", you may ask.
Racial discrimination is closely related to trauma, and can even cause Post-Traumatic Stress Disorder (PTSD).
It is, indeed, one of the greatest misconceptions about PTSD, that it’s limited to wars and combat
zones or to a life-threatening event. The reality is that one can have PTSD simply from witnessing a
traumatic event of any nature or even if a loved one has suffered a traumatic event. (A 2014
study from the University of Miami showed that almost 50% of women had PTSD
symptoms after Hurricane Katrina, for example).
The DSM- 5 even broadened the definition to include a person who learns about a traumatic event
that happened to a close family member or a close friend, and also stress due to a prolonged
exposure to an aversive situation.
Well, racism itself may be a traumatic experience!
Watching repeated acts of violence is a source of stress and trauma in Black people, particularly
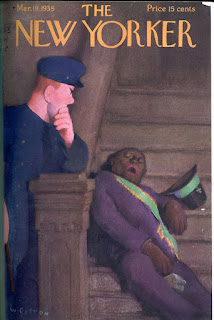
black women. Research has shown that stress and trauma from racially motivated events create
reactions that can be identical to PTSD.
If I am African American and I see this pattern on television I may identify myself with the entire
situation. But trauma extends well beyond what we see on cable news and social media. It is an
everyday challenge that people face with institutionalized racism leading to what some mental health
professionals call RACE-BASED TRAUMA. Racism continues to be a daily part of American
culture and to have an overwhelming impact on the oppressed.
In the case of racial discrimination, we’re not talking about an issue that’s been around for
years or decades, but centuries. It’s people who were kidnapped and thrown in the bowels of slave
ships and submitted to forced labor and torture. Later on, that was translated into exclusion from
educational, social and health resources causing disparities that are linked to mental health.
It's important to have that in mind in order to understand one's perceptions and society's
(mis)perceptions.
Victims can become distressed by things that are not typically worrisome to white people, for
example. "Microaggressions, or routine slights, can trigger stress reactions: it’s the black man
followed by a security guard at the department store or the white woman clutching her purse when a
black man enters the elevator", says Dr. Carl Bell, from the University of Illinois at Chicago.
What is PTSD?
It’s a severe and chronic condition that may occur in the aftermath of a traumatic event.
Symptoms usually develop within the first 3 months after the trauma and the diagnosis is made
if symptoms persist for over a month. Women are more affected than men.
Symptoms include depression, anxiety, flashbacks, fear, intrusive thoughts about the traumatic event, recurrent nightmares (leading to sleep difficulties), anger, apathy, inability to get pleasure, impaired concentration. It may also cause hypervigilance, hyperarousal and an exaggerated startle response (certain sounds or smells make the person relive the trauma) as well as avoidance behaviors leading to social isolation-- the person becomes more seclusive and uninterested, fears getting out of the house, or may change the route they normally take to avoid walking by a police officer or the street corner etc.
PTSD may have short-term or long-term impact. How long? The answer may be shocking:
Studies suggest that trauma is intergenerational and inherited, with memories passed along
through the DNA! That is shown, for example, in several interesting studies with families of
Holocaust survivors, or more recent studies with victims of the 9/11 attacks, that showed that
pregnant women who experienced the bombings passed on biological signs to their babies.
There is another study from Columbia University that revealed that one-third of NYC’s school
children suffered mental health disorders following the WTC attacks.
We must ensure black women have the ability and the right to raise their children in a healthy
environment. It is a matter of Reproductive Justice.
African-Americans are 20 % more likely to report serious psychological distress than adult whites;
they are also more likely to have feelings of sadness, hopelessness, worthlessness and more likely to
attempt suicide (8% vs 6%).
The National Survey of American Life found that AA have a prevalence of PTSD around 9% (vs
6% for Non-Hispanic Whites). In certain populations, this number can get much higher. Inner city
studies in high crime zones of Detroit and Baltimore show something like 30%, which is
comparable to war zones in Vietnam, Iraq and Afghanistan.
AA usually have more serious traumatic events and are more likely to experience child abuse,
sexual trauma, and to witness domestic violence. An Emory study showed that almost 90% AA
living in impoverished urban areas reported some form of trauma.
A UMichigan study from 2011 with 1600 women (~half AA) showed that the prevalence of PTSD
was 4 times higher among AA, but they were also less likely to get treatment. They also noted
the correlation of PTSD and pregnancy complications, including preterm birth (due to increased
cortisol levels causing placental abnormalities).
AA are under-represented in outpatient settings but over-represented in inpatient treatment.
They are also over-represented in jails: AA and Hispanics comprise 30% of the US population but
account for almost 60% of the prison population. They’re also 14% of drug users but 37% of
drug arrests.
Police are also at an increased risk for violent behaviors as a consequence of stress. The uncertainty
about whether they’ll come home alive to their families at the end of their shifts and the pressure
from being at the front lines may cause depression, and anxiety, and burnout. Stigma is particularly
significant in this population and a lot of them won’t disclose their feelings and struggles with fears
of being perceived as weak, or even of losing their jobs.
As a consequence, lot of them will use alcohol or drugs to self-medicate their symptoms, making the
symptoms much worse and more difficult to treat and contributing to poor judgement and
inappropriate defenses.
This attitude is thankfully starting to change but the process is really slow: There’s still something
between 120-140 documented suicides per year among police officers and a very high prevalence of
PTSD (1 in 8).
What can be done?
We need to understand this phenomenon as a Public Health Crisis: there are still a lot of underserved
areas and significant lack of resources to treat mental illness. AA physicians are 5 times more likely
to treat AA patients but the vast majority of mental health professionals are white.
Some people have difficulty expressing their feelings and experiences thinking they won’t be fully
understood. It’s important to make mental health professionals aware and
teach them how to address this problem and how to actively screen specifically for racial-based
trauma when assessing the trauma or abuse history.
Despite the growing evidence that PTSD is related to racial discrimination, little is being done to
address this problem. Hospital trauma centers are well-equipped to treat the physical injuries
from the trauma, but not its emotional and psychological components.
We have a number of evidence-based interventions and treatment models for trauma but not
specifically for racial trauma so more studies should be done and more attention should be paid
to this matter.
Also it’s important to develop interventions to decrease violent crime and increase access to
mental health treatment and to work on decreasing the stigma that surrounds mental illness.
Below is a panel that aired last week on the morning news about the theme of Race, Trauma and Urban Violence:













